Where do I find a doctor to prescribe female hormones?
This is probably the most common question from new gals wanting to go further with gender expression. Starting HRT is often the essence of declaring “I’m transsexual” to many gals.
HRT Realities for Transsexual Women
I doubt anything is less understood by beginning transgender females than HRT. Early-on in my own journey, I discovered part of this problem was rooted in the number of transsexual women that exaggerated what hormones had done for them versus certain cosmetic procedures which they didn’t want to own to having had completed. Alas, this is fairly common in the world of women. Most of my natal female friends prefer to keep any cosmetic adjustments a secret, as well.
Neophytes are sometimes told “hormones” caused my changes.
Additional chapters in This Section include:
MTF Transition Success: Making the Biggest Decision of your Life
MTF Transition - Detailed Guide
MTF Transition - Deciding to do it or Not
How Long Does it Take to Successfully Transition?
Hope for Anyone: What I looked like before transition
Hormone Therapy MTF Transsexuals
Myths of Hormone Replacement Therapy for Transgender Females
HRT is not a magic pill
It'll help. However, generally speaking its effect are subtle. It can create small breasts and larger nipples. It also mildly “softens” your face & skin tone from a more ruddy male presentation - but not in a monumental way. Regardless if you took testosterone or female hormones - it’s going to create consequential emotional mood swings you must learn to manage. Such outbursts can cause you to lose your job or loved ones. They’re not an excuse to hide behind your female journey.
HRT doesn’t eliminate facial hair
Sadly, HRT has littler no effect on facial hair growth. A blocker and estrogen regimen will tend to reduce body hair growth - but you’ll still need to deal with facial hair removal the old fashioned and painful way…sorry!
HRT doesn’t change your voice
Another big myth. Developing a feminine and passable voice is an essential skill for any transsexual woman. HRT isn’t going to help in this regard.
HRT doesn’t create hips
This is probably this biggest myth. You might see mild improvement in fat storage occurring in your ass after years of hormones and blockers - but the effect is minimal. It gets better in that regard a few years after GRS or an orchie - but it never “creates” hips. Your hip bone structure is installed at birth. Additional augmentation can be achieved from buttocks implants or certain injectibles.
HRT is not an excuse to be neurotic
Most every new gal literally relishes the incredible new feelings that occur from HRT. Emotional swings, etc. Unfortunately, it also tends to make us a bit incorrigible as we accentuate our experience – aka - the placebo effect.
All of this can have a horrible impact on our co-workers or loved ones. It’s never okay to have emotional outburst that affect others.
Impact of Hormone Replacement Therapy on Transgender Females
As I recall, Annie Richard’s site included the only definitive analysis on impacts from HRT I ever saw. My own observations are based upon my own experiences and those of lots of friends.
HRT will soften male facial features
Men usually have more rugged facial features than women. This is caused by facial hair, its related large follicles and much higher levels of testosterone. A long term HRT reigning softens this appearance to a more feminine look. It usually takes about a year until such results are very noticeable and results vary depending upon where you began in this scale as well as if you’ve begun electrolysis to remove facial hair and follicles. Taking testosterone blockers like spironolactone helps this process greatly.
HRT will create breast growth
You will most definitely see breast tissue growth from a combination of estrogen-based products and t-blockers. The actual size you achieve is based upon your own family genetics but your breasts will begin to form and your nipples will grow and become more sensitive to the touch.
Most gals grow into a full A-cup or small B-cup from HRT - which creates an ideal basis to install breast implants.
HRT will reduce physical strength
You will notice reduced physical strength from a combination of estrogen-based products and t-blockers within about a year. The most noticeable will happen from hand strength when you grip something tightly. However, you’ll also see a decline in sheer force.
This reduction doesn’t become complete until years following GRS or an orchie. T-blockers just don’t product the same results as removing “the source”.
HRT will often cause emotional swings
If you’ve not been in touch with your emotions “as a man” - you can expect to get a dose of that reality on a trans HRT regimen. Outbursts of anguish, crying and depression are often common. We essentially go through the “reverse process” of menopause compared with born-women.
You need to remain extra aware of this impact and not let it negatively affect your close relationships or career. There’s a bit of a placebo effect we often feel in this process along with real results as we “change”.
As I mentioned earlier, this is not an excuse to lose your job and loved ones.
The traditional path for getting on hormone replacement therapy for transsexual women
There’s a clear-cut path for a transgender woman to get legally prescribed hormone replacement therapy. It includes regular meetings with a certified counselor who determines via an established criteria if you are indeed a good candidate to start HRT and gear to transition your gender. THere’s a valid reason for this roadblock: transition isn’t about fantasy fulfillment. It’s an absolutely overwhelming life decision that often includes grave consequences. You should thus be very sure before you start down this path in earnest.
You can find a qualified gender therapist by searching on-line using such keywords as therapist, gender identity , transgender, transsexual, gender disorder, etc.
Some girls complain they can’t afford such counseling and thus are blocked from getting the HRT they need. I’m sympathetic to that plight - having once been completely broke and homeless - but I need to remind you that HRT is perhaps the least inexpensive item in a transition journey. Also, starting transition without a viable economic plan often results in a stalled transition - which can be worse than never transitioning at all.
Subsequent to this certification from a licensed therapist, you’re given a letter recommending you for an HRT regimen. Sometimes a therapist can guide you to an endocrinologist whose transgender friendly - sometimes you just have to find one on your own. Reaching out to transgender support groups on-line in your area is the best way to find a medical resource.
Hormone replacement therapy for transsexual women
There are two essential links you will want to bookmark and review as you consider starting HRT in concert with your transition. Dr. Anne Lawrence includes detailed regimens targets for your blood work - which can be used to help educate uninformed prescribing doctors. Annie Richards information details studies regarding anticipated changes to the male body from HRT
Anne Lawrence - detailed info on HRT regimens
Buying Female Hormones On-Line without a Prescription
I have a number of friends who completed transition through the use of non-prescribed HRT regimens. The most popular and reliable site for acquiring such meds is Transgender Zone:
Transgender Zone
The trickiest part with this path is the inherent dangers you face with blood clotting and related side effects from HRT - particular if you are a smoker. I’ve witnessed more than one transgender girl fall ill from this path from heart attack, stroke, and cancer.
Please be very careful!
Are you prepared to start your gender transition?
The primary goal of passing as a crossdresser is going unnoticed - being able to enjoy your time as a girl without others being aware you’re transgender. I spent about 70% of my time as a woman before transition and thought I was totally ready for transition.
I wasn’t.
Passing as a crossdresser is not the same as functioning seamlessly as a transsexual woman. Are you getting a bank loan for a new house in your dress? Are you closing a big new client at work while en-femme? Are you attending your family reunion in full makeup?
My biggest mistakes with not being fully prepared for transition? There were four - I’ll share here - as well as what I would have done differently. In other words? I don’t want you to repeat my mistakes.
Fair enough?
Embracing how long it would take
Functioning seamlessly as a woman, getting past all the local drama associated with your transition, becoming totally confident with your new self in all circumstances, establishing a new and healthy non-trans social sphere? These things take a long time - much longer than we would think.
The first big hurdle is getting past your transition being newsworthy to old friends and family. Often, when we first announce our intentions or go full-time - the event is “headlines” amongst past associations. Like all sensational stuff, it just takes time for the story to go from page A-1…to D-37. Essentially, it requires that everybody is now aware of it, at least a few friends meet you in your new gender - report back you look good and seem happy. You can make this process go smoother if you steer clear of creating drama in your new life - don’t engage anyone who makes snide comments early-on: just let it. This too, shall pass.
The other part that can make time seem to move more slowly is a sense of loneliness and isolation that’s common for trans-women. My mistake was thinking I could find solace in trans culture and friends as I did while a crossdresser. There really is no healthy “trans life” following transition. Most girls that live that way are doing so because they’ve yet to build a consequential life as a woman. I also made that mistake - don’t want you to repeat it.
It takes time to find and develop sincere close associations. I want you to invest that effort into real-time female friends that live nearby. Reduce contact with on-line trans friends. The former will enrich your life. The latter is often a source for self-perpetuating victimology and negative impulses.
Not first finishing electrolysis
I mention this repeatedly - and I’m going to keep harping about it. Why? Because almost ever trans-woman fails to get this completed before going full-time - and regrets that oversight. I jumped to heavy laser - figuring that would do the tick. It did…temporarily.
It’s a brutal, painful and expensive process. Get it complete before you go full-time and your journey will be much easier!
Not spending enough femme time doing mundane tasks and interactions
The most overwhelming tasks following transition are often the simplest. I mistakenly used most of my crossdressed hours with trans friends + going to dinner and having fun.
If you want to be ready?
You need to constantly go shopping, interacting and living as a girl leading up to your big change. I’m not talking socially: I’m talking mundane tasks. The key here is to gain more confidence with your demeanor, your voice and your personal style.
It's the little things that make the big difference!
Not establishing a viable economic plan for a gender transition
Successfully changing a gender is very expensive.
Just establishing an age and event appropriate wardrobe for all seasons is insanely costly - never mind the surgical investments for transition or the increased “chick costs” - like skin care and hair maintenance.
All this takes money - and lots of it. My mistake was thinking my newest deal was going to work out smoothly and fully fund these important changes. I underestimated the overwhelming emotional toll of transition - and its impact on my work productivity. The most successful economic transitions I witnessed were with girls that first saved for their changes and stayed in their present career - dealing with all the snide comments from old comrades.
Most of us would prefer the Cinderella approach - a fresh new start in our new gender where nobody knew the old male self. Alas, Cinderella was a fairytale. It takes a very long time to achieve that look and confidence we dream about.
Be realistic and courageous - and your chances for success improve dramatically.
The Final Analysis: The Most Important Prerequisites for a Successful Gender Transition
Okay, if I haven’t yet deterred you from going forward with transition, the least I can do is push you towards the right steps.
There are three essential prerequisites to moving forward and succeeding with a gender transition.
A Viable Economic Plan
Nothing is more important to completing transition than a viable means to earn a living during that process. As a reminder: an “all new” career just as you start your transition is not a viable plan. Neither is some new idea to sell goods and services to the transgender community. Trans-world is very small: there’s not much money to be made within it.
You are blessed. Like never before, company’s maintain policies in support of transgender women. That doesn’t mean you won’t face a new invisible ceiling on advancement. It also does’t mean you won’t face some ugly comments. However, it’s more doable than ever.
A gender transition is expensive. Its time consuming. It’s exhausting. You can’t successfully undertake a project like that - if you’re constantly worried about paying rent or how you’ll pay for your next meal.
No matter how neurotic you might feel after starting HRT. No matter how frustrated you might become over people’s lowered impression of you - don’t quit your job or provide a valid reason for them to fire you. It’s crucial to be employed to succeed at a gender transition.
Dealt with your major nightmare
Everybody’s got that “one big nightmare” they must overcome in order to make transition a success. Could be dealing with your parents - or your spouse. Could be getting a job with an HRC sensitive policy or completing electrolysis. Whatever your big dilemma? Deal with it head-on before you start this journey. You’ll face all kinds of minor obstacles throughout transition. Don’t leave a “major” condition on the table, as well.
Embraced how long it’s going to take
It’s ten years: period. Don’t care how much money you have or don’t. Don’t care what your circumstances - plan on it taking ten years until you’ve completely transitioned and established the sort of quality of life you once knew before at every level - and that’s if this goes well.
Don’t harbor any “Cinderella” fantasies about going away and coming back a beautiful girl where nobody knows your a transsexual. Not going to happen and that mindset only sets up frustration.
Female Hormones
and the transsexual Women

Important Disclaimer: This page was established to help inform transgendered women when I was making life changing decisions. I'm not a medical professional and the content does |
NOT
constitute Medical Advice. I disclaim any responsibility for extracts that have appeared elsewhere that might imply that it does. Also, I cannot accept any responsibility for any medication that a reader may take. Such treatment should always be done done under the supervision of a qualified medical professional.
|
| Introduction to Hormones |
|
All animals have hormones. Hormones are chemical messengers that travel through the blood and turn body functions on or off. For example, some hormones tell your heart to beat faster when you get scared while others control fat deposition. Hundreds of hormones are in our body's, carrying many different messages.
|
For male-to-female transsexual women, taking hormones becomes part of their daily routine. Although the amounts taken can be reduced after sex re-assignment surgery, it will still be necessary for them to take hormones every day for the rest of their lives in order to remain healthy. It must be emphasized that some of the effects of long term hormone use are irreversible, at least without surgery; hormones are not something that can be experimented with. The widely followed
HBIGDA Standards of Care of Gender Identity Disorders
Version 6, warns that:
|
"Social Side Effects [of Hormones]. There are often important social effects from taking hormones which the patient must consider. These include relationship changes with family members, friends, and employers. Hormone use may be an important factor in job discrimination, loss of employment, divorce and marriage decisions, and the restriction or loss of visitation rights for children."
|
Before taking female hormones it is also necessary to carefully consider several other important points:
|

Many girls have over-
optimistic expectations about the effects of hormones.
|
Firstly, why do you really want to start taking them? The results of prolonged use of hormones such as estrogens at medicinal levels are
obvious and permanent
. Taking female hormones makes no sense unless you are seeking permanent and irreversible body feminization. In particular breast development can soon become a source of embarrassment for some one still living as a man, it will not shrink significantly when the hormones are stopped, and may eventually require surgical removal (gynecomastia).
|
Secondly, there are serious
medical risks
associated with long term hormone use, although admittedly recent studies seem to show that these risks are much less than previously thought, for example post-operative MTF women seem to be no more at risk of getting breast cancer than genetic women on HRT.
|
Thirdly, there are
considerable costs
associated with hormone treatment, particularly if "natural" hormones are preferred over much cheaper "synthetic" hormones which are thought to have higher risks of side effects and complications. The cost of hormones varies hugely from country to country, but if you are paying yourself then $100/€100 a month is about the minimum budget for hormones and anti-androgens when pre-SRS, perhaps halving after surgery. This may not sound too much, but it must be maintained month after the month, and the total annual expenditure can be a significant burden, particularly for young women on low salaries and pensioners.
|
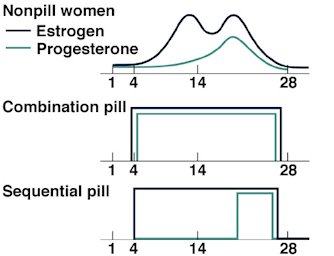
The crazy monthly hormone cycle of a fertile woman.
Finally it is necessary to
be realistic
about what feminizing hormones can do, they are not some magic potion. Also the effects take a long time to realize - it's at least two to three years before maximum effects are achieved.
|
Types of Hormone
Oestrogens
Oestrogen (or 'Estrogen' in American English) is the most important female hormone taken by transsexual male-to-female women.
|
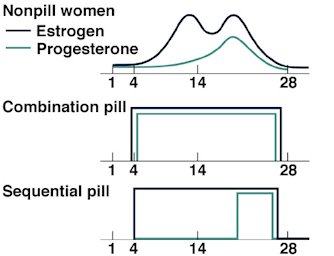
Many transwomen try to emulate the estrogen and progesterone cycle of women, but most eventually give up - thus avoiding the associated mood swings, hot flushes and physiological effects.
|
Estrogen's are steroid "female hormones" produced in large quantities by the ovaries of women, however they are also produced in small quantities by the testes of men. During a girl's puberty it's a flood of estrogens that are responsible for the development of female secondary sexual characteristics such as breast enlargement, broadening of the pelvis and fat deposition around the hips. In a sexually mature woman with female reproductive organs, estrogens participate in the monthly menstrual cycle that prepares the body for a possible pregnancy, and they also participate in the pregnancy if it occurs.
|
Estrogens also have several non-reproductive effects: they are mental tonics and have anti-depressive effects; they antagonize the effects of the parathyroid hormone, minimizing the loss of calcium from bones and thus helping to keep bones strong; and they promote blood clotting and may lower the risk of heart disease (although a recent study has questioned this) .
|

In terms of the specific biochemicals contained in estrogen-based hormone preparations, there are three main categories of interest to transsexual women:
|
| conjugated estrogens - from natural sources e.g. Premarin, from pregnant mares’ urine. |
| estradiol valerates - synthetic copies of vegetable (yam or soya) estrogen. |
| phyto-estrogens - from plants, e.g. Ogen. |
|
For hormone therapy both synthetic and natural estrogens are commercially available. Synthetic estrogens are generally cheaper but more prone to side effects than are natural estrogens. Products based on phytoestrogens are available in health food shops but are not subject to licensing or standardization of their active constituents, and are usually of
very low
, and possibly ineffective dose - the sweeping claims made by manufacturers of such products should treated with great skepticism.
|
Most of the preparations that are licensed for use as female hormone therapy (these may be conjugated estrogens, but are usually based on estradiol valerates) are only available by doctor’s prescription. Estradiol valerate is the only form of hormone therapy that can be measured in blood, so blood estrogen measurements are meaningless in someone taking, say, Premarin.
|
Progesterone
Progesterone is another steroid "female hormone". It is secreted by the corpus lutetium and by the placenta, is responsible for preparing the body for pregnancy and if pregnancy occurs, maintaining it until birth. Progesterone is very important during pregnancy and pregnant women have lots of progesterone, which helps their bodies support the developing baby. It is also known that progesterone has an effect on the brain, where it acts as a mild anesthetic.
|
There was once a debate about whether transsexual women needed progesterone, given that they do not have a uterus (lowering the risk of uterine cancer is usually the main reason for including progesterone in HRT in women). However it now seems probable that apart from its obvious effect on the uterus, progesterone has many effects on other tissues in the body, some having nothing to do with sex and reproduction. The current medical consensus is that progesterone is important since it is obviously part of the general hormonal cocktail in XX women, thus transsexual women are now recommended to take progesterone along with their estrogen.
|

In the transsexual woman progesterone administered with estrogen appears to help promote breast growth: estrogen stimulates cell mitosis and growth of the ductal system, while lobular development and differentiation seems to be dependent on progesterone (breast fat accretion seems to require both). Progesterone consistently administered with estrogen also seems to reduce the risk of fibrosis, cysts, and cancer from administration of estrogen alone.
There are some prescription HRTs available that are based on synthetic progestogens (chemicals that have progesterone-like actions), e.g. Provera and Duphaston. True, non-synthetic, progesterone (as opposed to a progestin) is very rarely reported to have any adverse effect, and seems to provide a healthier balance for an aggressive oestrogen dosage in pre-op TS women, as well as improving libido and overall energy level.
|

Gia and Allanah posing as sisters after after many years on hormones (plus lots of surgery!)
Androgens
The principal androgen (male sex hormone) is testosterone. This steroid hormone is mostly manufactured by the interstitial (Leydig) cells of the testes and therefore men have much more testosterone than women. Testosterone is one of the hormones that make men look different from women, secretion of testosterone increases sharply at the start of a boy's puberty and this is responsible for the development of the male secondary sexual characteristics such as beards and deeper voices. Testosterone is also essential for the production of sperm by men.
|
|
One of the well-known effects of testosterone is that it stimulates muscle growth. For this reason, some athletes and body builders (both male and female) take testosterone or similar drugs - called "anabolic steroids" - to help them build bigger, bulkier muscles. Conversely in pre-SRS transsexual women it is highly desirable to block the muscle building and other masculinizing effects of androgens such as testosterone which are produced by the testes, and to a lesser extent the adrenal cortex. This can be most safely and effectively fought by taking an "anti-androgen" drug, rather than by trying to overwhelm the effects of androgens by mega-dosing with estrogen. The Spironolactone and Finasteride anti-androgens are very commonly prescribed and taken by pre-SRS transwomen, transsexual women older than 25 or so seem to find taking an anti-androgen to be much more effective and important than those who are younger. Most post-SRS transwomen don't need an anti-androgen, but a few find Finasteride to still be useful.
|

Gonads
The gonads (ovaries in women and testes in men) are the reproductive organs which produce eggs and sperm, the cells that join to form an embryo that develops in to a baby. Gonads also make most of the reproductive or sex hormones produced by a body. Testes produce testosterone while ovaries produce a mixture of estrogens of which estradiol is the most abundant (and most potent). These hormones are necessary for the growth of eggs and sperm, but in addition they are responsible for the development of many of the characteristics that make men and women look different from each other (the so-called secondary sexual characteristics).
In a transsexual woman the surgical removal of the testes either during sex re-assignment surgery or by a bilateral orchidectomy (castration) is highly desirable because of the virilizing effects of the testosterone they produce. Without the testes present, not only can smaller doses of female hormones can be administered but unopposed by testosterone this will often have a greater feminizing effect on the body than before.
Puberty
Puberty is largely initiated and controlled by the sex hormones.
Puberty can be defined as the biological developments which change boys and girls from physical immaturity to biological maturity, and many of the differentiations in outward appearance and body shape between men and women occur or develop further during puberty. Unfortunately for a male-to-female transsexual, an inappropriate male puberty sets a physical mountain that can never be full conquered.
A lot more information about puberty and its effects is given in the separate
article which can be found here.
|
|
Oestrogen can be taken in pill, injection, or skin patch (shown) form.
Effects of Hormone Treatment
A post male puberty male-to-female transsexual who commences female hormone treatment is effectively triggering some aspects of a second, female type, puberty in her body.
|

Professor Marie-Pier Ysser, formally the showgirl "Bambi". Shown age 40, after 20 years on hormone therapy.
|
In general, the increased estrogen and progesterone blood levels resulting from the female hormone treatment will stimulate and promote the growth of female secondary sexual characteristics (breasts, fat distribution, pubic hair pattern, ...).
Body shape
is controlled by estrogen so its use stimulates a female body shape to develop, and the woman's body shape and "figure" will become far closer to female norms in proportions.
|
The effects of female hormone treatment will vary considerably by individual, and can take 2 to 5 years to fully achieve. In order to maximize the physical effects and benefits, hormone treatment should be begun as
young as possible
, before the body has completely matured and can no longer develop in response to stimuli. Maximum feminization occurs if hormonal treatment begins before a male puberty.
|
|
|
|
|
If the testes have been removed in infancy or early childhood (usually because the child has been identified as
|
intersex
or
AIS
, and a female gender has been agreed with the parents), hormone therapy is usually started at the age of about 10 or 11, in order to initiate a female puberty. Unfortunately of course this ideal situation is very rare - the average 'western' transwoman is in her 30's before she commences hormone treatment. If a male puberty has already occurred, whilst female hormone therapy will cause a reduction in the levels of 'male' androgens such as testosterone, this will have little or no effect on most of the already developed of male secondary sexual characteristics (e.g. deepening of voice, facial hair, narrow pelvis, ...). The longer after male puberty (which typically ends by age 18) that female hormone therapy is started the less effective it will be - but not on a linear scale, the effects tail-off rapidly as time since puberty increases. For example, a woman starting hormones at age 20 may experience good breast development and a near cessation of facial hair growth, the same woman starting treatment at 30 will get considerably less breast development and only a slight reduction of facial hair growth, while if she started at 40 the effects will be less again, but not so significantly.
|
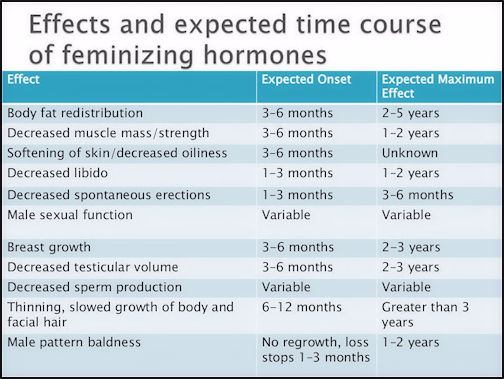
The following table shows the effects of female hormone treatment begun after male puberty has completed (i.e. after about age 17).
|
|
Desired Characteristic
|
Effects of
Hormone Treatment
|
Possible or Additional Treatments
|
Female type skull shape and facial features
|
|
None
|
|
Feminisation of jaw, brow ridges and skull possible via surgery
|
Softer, clearer skin with no acne or spots
|
|
Considerable improvement
|
|
Deep chemical skin peel
|
Smaller teeth
|
|
None
|
|
Dental surgery to improve teeth
|
Smaller nose
|
|
None
|
|
Rhinoplasty surgery
|
Smaller hands and feet
|
|
None
|
|
None
|
Reduce height
|
|
None
|
|
None
|
Broader pelvis
|
|
None
|
|
None
|
Stop facial beard hair growth
|
|
Little or no effect
|
|
Electrolysis and laser treatment
|
Thick female type scalp hair and forehead hairline
|
|
Hair loss ceases, slight reversal of balding
|
|
Wig, hair implants, some medications may help
|
Develop female pubic hair pattern. Hairless trunk and limbs.
|
|
Substantial improvement after prolonged treatment
|
|
Electrolysis and laser treatment
|
Higher pitched feminine voice
|
|
None
|
|
Voice training, voice change surgery
|
Reduction of "Adams Apple"
|
|
None
|
|
"Tracheal Shave" (thyroid cartilage reduction) surgery
|
Slimmer neck
|
|
No effect not ascribable to dieting
|
|
None
|
Breast development
|
|
Variable, from slight to substantial breast development (Note 1)
|
|
Mammoplasty
(breast implants)
|
Female type subcutaneous fat deposits (particularly thickening of hips, buttocks & thighs) and body shape.
|
|
Variable, slight to substantial fat redistribution after prolonged treatment
|
|
Fat transfer, implants
|
Reduced weight
|
|
Weight increase (Note 2)
|
|
Liposuction, diet and exercise
|
Small waist
|
|
May actually increase unless supported by dieting and exercise
|
|
Liposuction, lower rib removal, diet and exercise
|
Reduced muscular development
|
|
Some reduction
|
|
None
|
Reduce size of penis and testes
|
|
Substantial to significant reduction(not necessarily good if SRS is planned)
|
|
Surgery
|
Good mental health
|
|
Depression may occur
|
|
Therapy, support of friends and family, anti-depressants
|
Menstrual cycle
|
|
PMS and Hot Flashes only (Note 3)
|
|
None
|
|
Hormones can't alter the skeleton of an adult transsexual woman, but can help soften and feminize the detail.
|
Notes:
1.
Breast development
will vary considerably depending on the individuals genetic make-up and the time from puberty. Early hormone treatment (by age 18) will typically result in breasts about one bra-cup size less than the girl's mother and sisters.
|
2. Oestrogen hormones help to deposit fat. On a male type skeleton this can result in weight gain and a larger rather than reduced waist line. Sensible
dieting
and suitable exercising (e.g. aerobics, not power lifting!) is essential for developing a female type figure and body shape.
|
3. Periods and menstruation are impossible even for a post-SRS transwomen. However most transwomen will suffer from Pre Menstrual Syndrome (PMS) and Hot Flashes if they choose to stop taking oestrogen for 1 week in every 4 week period. These unpleasant effects can be avoided by maintaining a continuous hormone dosage.
|

Continuous female hormone treatment at the levels recommended for a MTF transsexual will make the penis incapable of an erection and ejaculation within 4-6 weeks.
|
Maintaining Male Libido
The taking of significant amounts of female hormones by a man will reduce his sexual "potency" to zero within two or three months. The long term use of hormones inevitably means a greatly shrunken penis, an inability to have erections, and permanent infertility after perhaps two years. However for various reasons some male-to-female transsexuals wish to preserve their ability to have a penal erection, sexual intercourse and ejaculate, whilst still feminizing their body. This is rather a contradiction but stop-start hormone treatments and the use of drugs such as Viagra can result in a compromise for a few years.
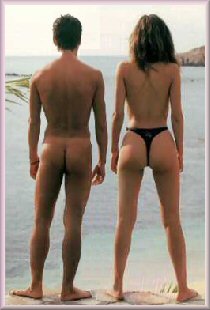
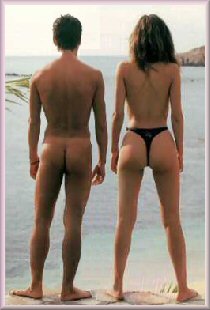
 "Female" type fat deposit areas
"Female" type fat deposit areas

Nikki began hormones in her mid-teens, 20 years later her female type fat distribution is evident.
Weight, Muscle Loss and Fat Re-Distribution
One very visible effect associated with the long-term use of female hormones by a male-to-female woman is changes to her fat distribution and muscles - and thus to her appearance.
In one
study
, profound changes in weight and fat distribution were observed in 20 MTF transsexuals after taking hormones for just 12 months. A marked increase in subcutaneous fat deposition was observed, reaching near female norms in the arms, abdomen, hips, thighs, etc. Other
studies
support these findings. It's also become clear that transsexual women on hormones loses muscle mass, in particular there is likely to be a large decrease in thigh muscle, instead a considerable subcutaneous fat deposit is accumulated in this area - this is a typically female characteristic as the thigh is not a primary site for fat storage in men.
Transsexual women often have great legs. When softened by the additional fat deposits resulting from female hormones, the long legs of a genetic male can have a serious "WOW" factor. Big feet can actually enhance the affect when wearing high heels.
|
As well as hormones, a doctor may be able to recommend other drugs to aid fat redistribution and weight control. One such drug is Metformin (one brand being Glucophage). Although normally associated with diabetes, it's now also considered useful for aiding and enhancing the body fat redistribution (including limbs and face) of transsexual women taking estrogen.
Despite a loss of several kilogram's of muscle mass, adult male-to-female transsexuals actually have a tendency to gain weight after starting hormones as they put on so called "reproductive fat". An overall gain of 4-5kg (10-12 lbs) seems typical - the largest fat deposition occurs on the hips and thighs, with a typical gain of 4-5 cm (2 inches) in hip measurement. Whilst there are far smaller deposits on the abdomen, this can still result in a 2-3 cm (1 inch) increase in waist measurement - with unfortunately little net improvement in the waist-hip ratio (WHR), a key physical "female indicator" that's subconsciously observed by other people.

Hormones, a good diet and exercise will radically change a transwoman's body, but a male-type skeleton can't be totally hidden.
|
The problem for most transwomen is that their underlying male type skeleton is differently shaped from genetic woman, and thus achieving phenotype female fat deposits will not still result in a hour glass or even pear-shape figure. Some transwomen do attempt to compensate for this fundamental problem by augmenting the size of their hips and buttocks with butt implants or even dangerous silicone injections. Liposuction body contouring is another common quick-fix option used by many transwomen these days; however, it is not a substitute for weight reduction - particularly in an obese individual.

In the west, nearly half of transgendered women only begin hormones age 40+. The picture shows a 58 year old after 2 years treatment.
|
The tendency of male to female transsexuals to gain weight is best countered by appropriate exercising and dieting. This will assist and magnify the effects of drugs in developing a female type figure and body shape - a moderately active metabolism means that typically "male fat" on areas such as the stomach will be burnt up while female-type fat on areas such as the buttocks will still be deposited.
Exercising should emphasize burning calories and general toning rather than aim to maintain or even increase physical strength, so daily sessions of aerobics, swimming or cycling are appropriate, but not power lifting, weights or even circuit training. Happily, once lost, it is almost impossible for a transsexual women to regain excessive "male" type muscle in areas such as the biceps if post-SRS or taking hormones and anti-androgens.

Transgender artist
Zackary Drucker
has photographed the evolution of her body since beginning hormones and transitioning age 23. Shown age 30.
|
After transition most MTF women reduce their calorie intake by a huge amount - perhaps a third based on limited evidence. Given the difficulty of long term dieting, the success of transsexual women might be an interesting area of study!
After perhaps an initial period of rigorous restriction (Atkin's et al), dieting really means a permanent change of eating habits, the aim is simply to adopt a healthy balanced diet that's relatively low in fat (this is easier to type than do, as I know!). A good rule of thumb is to eat no more than 2000 calories per day, if you are big framed then a better basis is fifteen times your
ideal
body weight (e.g. 140 lbs x 15 = 2100 calories); if you are exceptionally active then a few hundred extra calories a day may be appropriate. Avoid excessive long term dieting which becomes an eating disorder with malnutrition and osteoporosis. This triad may result in irreversible bone loss, psychological abnormalities and death.

A young transwoman with female type fat deposits on her hips, buttocks, thighs and legs. This is an unusually good result that may have been aided by surgical implants and/or silicone injections.
|
While female-type peripheral fat deposits on the bottom, legs and arms are not closely associated in women with increased health risks (heart disease, diabetes, ... ), excess fat around the waist is -
strongly
. Thus shifting fat from the waist to elsewhere in the body is win-win situation for the transsexual woman. Basically a good figure is a healthy figure, which is why women with good figures are more
attractive
to men!
The final objective should be a weight close to a female rather than male norm for your
height and build
(it is necessary to accept that most transwomen are physically more heavily built and thus heavier than genetic women of the same height), and a WHR of about 0.8. Unfortunately the underlying constraints of a male type skeleton make figures with a WHR of 0.7 or less very rare in transwomen.
Attractiveness
Women with high levels of estrogen tend to benefit in terms of attractiveness from a facial appearance aspect - healthier looking, fuller lips, better skin quality, less unwanted facial hair, etc. However good makeup and 'facial maintenance' can achieve the same - and thus totally negate these advantages.
Reality Check Time
|
|
Some women choose to begin hormone therapy for what may be the wrong reasons, and perhaps with unrealistically high expectations of what the results will be. It's essential to be realistic about what hormones and feminisation surgery can do. Many of the transsexual woman featured in magazines, newspapers, on talk shows, and other media are exceptional in their looks, and would probably very feminine without any hormones or surgery. Beautiful women are [mostly] born so, not made.
|
|

The left hand picture is perhaps OTT, but the reality is that gorgeous and totally passable transsexual women such as |
Ha Ri-su
(right) are the lucky exceptions, not the rule... perhaps rather more typical in appearance are the two ladies below whom I tried to randomly
select:
|

(Left) Judith Kerr, once John Kerr, and (above) Susan Watson, once James Watson
There are many support sites for the Transgendered that you are worth check out if you are considering hormones. Browse the pages of Miss Vicki Rene's popular "
The Prettiest of the Pretty"
website and objectively consider some of the women featured. Look for someone with similar build and features to yourself. Are you really likely to be a beautiful swan or an ugly duckling?
|

Two composite female faces without makeup, the left is
with high oestrogen levels and the right with low.
No Miracles
The visible changes in physique and appearance resulting from female hormone treatment can vary from dramatically successful to rather disappointing. However it is important to remember the limitations of hormones - they cannot change a
skeleton
, nor can they reverse aging. For example the pelvis of an average adult woman is significantly different from that of an average adult man - with effects which range from gait to appearance in a G-string - and these can't be overcome by hormones, or even with dangerously drastic measures such as silicone injections.
Hormones can greatly assist the transition of a short and lightly built young man in to a completely passable woman, but hormones (nor anything else) cannot turn a tall, rugged, heavily built, balding, and elderly man in to a pretty and petite girl. Such a man is always going to have difficulty passing successfully as a woman, indeed even after all available hormonal and surgical treatment, the brutal reality is that he may still appear to strangers as a man in drag with "boobs stuck on".
Modes of Delivery
There are five ways of taking hormones:
| transdermal (skin patch or cream/gel) |
| implant (pellet inserted under skin) |
| injection (e.g. intramuscular testosterone) |
| vaginally (cream or tablets) |
|
The doses provided by skin patches, implants and injections are lower than those of tablets because they do not involve the hormone passing through the liver - where a significant amount of an orally administered hormone will be metabolized and lost. So it is possible to directly compare the headline dosage figures on the packets. Vaginal estrogen preparations are not a source of whole-body hormone replacement, but help to treat vaginal dryness and assist with dilation in post-SRS women.
Hormone Therapy Products
There are a lot of hormone products on the market and finding the right one can be difficult. The questionnaire for The Million Women Study lists the following common UK preparations:
Prempak C 0.625 mg
Prempak C 1.25 mg
Tridesta
Trisequens
Trisequens Forte
Cycloprogynova 1 mg
Cycloprogynova 2 mg
Estrapak
Estracombi
Climaval 1 mg
Climaval 2 mg
Premique Cycle
Premique
Nuvelle
Kliofem
Livial
Premarin 0.625 mg
Premarin 1.25 mg
|
Evorel 25 mcg/50 mcg
Evorel 75 mcg/100 mcg
Progynova 1 mg (skin patch)
Progynova 2 mg (skin patch)
Estraderm 25 mcg (skin patch)
Estraderm 50 mcg (skin patch)
Estraderm 100 mcg (skin patch)
Zumenon 1 mg
Zumenon 2mg
Ethinyloestradiol (BP tablets in a bottle)
Micronor
Oestrogel (skin gel)
Provera (progesterone)
Duphaston (progesterone)
|
What suits one person will not suit another. There are really no guidelines other than just to keep trying different preparations until you find one that suits you.
|

Hormone Regime's for Transsexual Women
|
Many options for estrogen therapy exist for use in hormonal reassignment therapy, and the doses used are generally at least 2-3 times higher than doses used for hormone replacement therapy in postmenopausal women. Oral estrogen, either ethinyl estradiol (Estinyl) or conjugated equine estrogen (Premarin), is the most commonly used formulation, as it is relatively inexpensive. Transdermal estradiol patches (e.g. Alora, Climera, Esclim, Estraderm, Vivelle, Vivelle-Dot) are strongly recommended for transgender women who are heavy smokers and those older than 40.

|
Anti-androgen agents are often used in combination with estrogens in hormonal reassignment therapy to further decrease male secondary sexual characteristics. These anti-androgen agents presumably exert their action by lowering serum testosterone levels and by blocking testosterone binding to the androgen receptor. Effective agents include spironolactone, progesterone, testosterone uptake inhibitors, growth hormone releasing antagonists, and cyproterone. Potential benefits include mild to modest breast development, the softening of body and facial hair, decreased progression of male pattern baldness, and decreased erections.
|

For a comprehensive consideration of typical hormone regime's for transsexual women I doubt if there is a better resource on the web than the
article
on Dr Anne Lawrence's
Transsexual Women's Resources
site.
Hormone Replacement Therapy after SRS
When the testes are removed (orchiectomy, gonadectomy) during Gender/Sex Re-assignment Surgery or a bilateral orchidectomy (also known as gonadectomy) is performed, immediate long-term female hormone replacement therapy (HRT) is needed in order to prevent menopausal symptoms and to protect the skeleton from osteoporosis. Clearly transwomen should follow the advice of their physicians regarding post-SRS HRT, but as a guideline, the National Osteoporosis Society (UK) advises that the minimum daily dose to maintain bone density in normal adult post-menopausal women is thought to be 0.625mg conjugated estrogen (e.g. Premarin) or 2 mg estradiol by mouth, or 50 micrograms estradiol skin patch.

Finding the right dose is a matter of balancing symptomatic relief (hot flushes, mood problems etc.) and osteoporosis and cardiovascular protection, against the risks such as breast cancer that are often associated with higher dosages.
Potential Risks
The taking of female hormones by a male-to-female transsexual has associated risks which can in extreme cases be
life threatening
.
Side Effects
The "
Standards of Care"
states that:
"The administration of hormones is not to be lightly undertaken because of their medical and social risks. ..... cigarette smoking, obesity, advanced age, heart disease, hypertension, clotting abnormalities, malignancy, and some endocrine abnormalities may increase side effects and risks for hormonal treatment. Therefore, some patients may not be able to tolerate cross-sex hormones. However, hormones can provide health benefits as well as risks. Risk-benefit ratios should be considered collaboratively by the patient and prescribing physician."
|
When considering the use of female hormones, absolute and relative contraindications (undesirable conditions) must be considered. Absolute contraindications which should prevent the commencement of female hormone treatment include:
| Thrombophlebitis or thromboembolic disorders |
| Cerebro-vascular or coronary artery disease |
| Undiagnosed abnormal genital bleeding |
| Benign or malignant liver |
Relative contraindications which increase the risk of complications developing include:
|
Once on female hormone treatment, development of any of the following conditions should cause the transsexual woman to immediately seek the advice of a physician. These contraindications include:
|
| Carcinoma of the breast (Breast Cancer) or other oestrogen-dependent neoplasia |
As with any medication if you notice unexplained changes in your health notify your physician. The woman should report to her physician immediately the occurrence of nausea, vomiting, breast lumps, abnormal bleeding, leg cramps, water retention, headache, dizziness and light-headedness. Cigarette smoking is known to increase the risk of side effects with synthetic estrogens, and this may also occur with natural oestrogen.
The risks of complications developing can be |
significantly
reduced by leading a healthy lifestyle, for example:
| Drink alcohol only in moderation |
| Take the minimum hormone dosage necessary to achieve/maintain benefits |
Long Term Risks
There is only very limited information based on direct studies about the risks transsexual women face due to the long-term estrogen and progesterone based hormone therapy. Assumptions have generally been for the worst, but that is gradually changing as additional relevant research slowly appears.

Medical opinion has long been that the very high levels of hormone therapy required in a pre-SRS woman who has not had an orchiectomy will inevitably be associated with health risks in the long term - more than two years - and that these risks increase with the age of the patient (particularly if over 40). SRS or an orchiectomy allows a radical reduction in hormone intake, indeed the endocrinology and hormone regimen of post-SRS women is very similar to post-menopause women on HRT, however transsexual women who had SRS at an early age have the complication of needing to take HRT for a very much longer period of their lives than most women, so unknown side effects may yet emerge.
The news seems to be improving but is often contradictory, for example
one large scale study
found no evidence that transsexual women taking hormones are likely to die any younger than the general population, but
another
found that their mortality rate increased.

Hormones help young MTF transition'ers immensely in terms of achieving a female appearance, but surgery such as breast implants is still often sought.
|
In addition to the primary feminization effects, it now seems that long-term estrogen therapy may actually have some benefits for the body of the male-to-female transsexual woman. The very limited research available seems to show that post-SRS transsexual women are no more at risk of breast cancer then genetic XY women on HRT. But the evidence is unfortunately slightly contradictory - some research on transsexual women indicates that long term estrogen-based hormone replacement therapy (HRT) protects the women against heart disease but slightly increases the risk of breast cancer, while other research
suggests
that provided they are conservatively treated with estrogens then they may actually may run a smaller risk of breast malignancy than genetic females because the mamma-genesis (breast development) is initiated later in life.

Two reports published in the
Journal of the American Medical Association
on 3 July 2002 unfortunately contained some bad news. A study of 16,600 genetic post-menopause women taking a combination of conjugated estrogen (e.g. Premarin) and medroxyprogesterone acetate (a progestin, e.g. Provera) had found that HRT did lower the risk of hip fracture, a measure of osteoporosis, but it raised the number of strokes by 41%, heart attacks by 29%, and breast cancer cases by 26%. It should be pointed out that the overall risk of these events is still low absolutely, the figures represent for every 10,000 women taking HRT about 7 extra heart "events", 8 more breast cancer cases, and 8 more strokes per year. The estrogen-progestin combination was developed because taking estrogen alone was shown to increase the risk of ovarian cancer; however one report effectively recommended that genetic women who have had a hysterectomy (i.e. their uterus removed) should consider taking estrogen alone - this of course also applies to all post-op transsexual women.
Other Health Considerations
A post-SRS transsexual woman on hormones is far closer to a natal woman than a man where health matters are concerned. A few examples:
Breast cancer is serious risk - regardless of whether this is slightly greater or less than natal women. A mammogram every two years is essential for under 50's, and annually for over 50's.
|
A transwoman must regularly examine her breasts for odd lumps, secretions from the nipple, and changes in the shape of one breast.
|
Whilst a transwoman can't get cervical cancel, if she is sexually active she should still get a Papanicolaou test (aka Pap or smear test) every two to three years to identify abnormal conditions and infections
|
A bi-annual vaginal examination is recommended to detect growths or other abnormalities
|
Many transwomen suffer from vaginal irritation and malodorous vaginal discharge
|
Urinary tract infections are common, particularly if sexually active
|
An [apparently] greatly increased likelihood of suffering from fibromyalgia - a condition resulting in muscular pain and genera fatigue - which is rare in men
|
Osteoporosis - weakened bones and increased risk of breakages - is more likely
|
A significantly increased likelihood of suffering from migraines (x3 according to one study)
|
Drastic mood swings and depression (which had never been experienced by the suffer before SRS)
|
An [apparently] slightly increased risk of arthritis.
|
Unfortunately much of the above is anecdotal or accepted 'wisdom' Hopefully the long-term study (20+ years) of a statistically significant numbers of post-SRS transwomen will eventually provide good information - and without confusing contradictions between one report and another.
Another very serious problem for transwomen is the reluctance of GP's in the UK and Ireland to treat a patient when they discover that she is post-operative transsexual. In Ireland, (based upon personal experience in 2009), no health insurance company will accept a new customer who is a post-SRS transwoman.
Example Hormone Regimes
|
Warning:
Some of the hormone regimes stated below seem to be excessively high, overdosing on hormones will not have any additional physical feminization effects but does have
very serious and dangerous health risks
. Hormones should only be prescribed and taken under qualified professional supervision.
|

Leora Moore
Pre-SRS
Daily: 8 mg Estrofem
0.5 mg Dutasteride
200 mg Spirolacatone
200 mg Microgest (1st 10 days of the month)
|

Rachel Saunders
Pre-SRS
Daily: 1.25 mg Premarin.
|

Natta Klomklao
Pre-SRS:
Diane 35
|
Post SRS:
Daily: Premarin and 10mg estradiol valerate
Weekly: 250mg hydroxyprogesterone-Caproate injections
|

Julie
Pre-SRS:
Initially:
Daily 10 mg Permarin; Weekly injection of 300 mg spiro, proscar and prometrium.
Currently:
Daily 2.5 mg Premarin Weekly: injection of 1CC of 40mg per ml of Del-estrogen
|
Jhenna Kelly Taylor
100mg Androcur & Estradam daily.
|

Barbie
Pre-SRS:
Twice monthly injections of 40 mg Estradiol Valerate and 150 mg Depo-Provera.
|
Nun Umdomsak
Pre-SRS:
Diane 35 tablet & 1.25mg Premarin daily;
|
Post SRS
:
10mg Progynon Depot & 250mg Prolution Depot combined injection.
|

Vanessa Lopez
|
Pre-SRS:
Premarin.
|
Post SRS:
1 mg Androcur every second day.
|

Jessica
Pre-SRS:
2.5mg Premarin/day
10mg/ml IM (shot) weekly Estradiol Valerate (40mg/ml month)
300 mg Spiro/dy
Post-SRS:
0.65 Premarin daily
10mg/ml Estradiol Valerate every 10 days (30mg/m
o)
|

Kira
Post-orchiectomy:
1ml Estradiol Valerate injection monthly
|
Obtaining Drugs without Prescription
In the early 'naughtiness' it was very easy to obtain hormones - often quite cheaply - over the internet without a prescription. Most countries require a doctors prescription for the purchase of female hormones and anti-androgens from a local pharmacy. However the importation of prescription medication is actually legal in many of the same countries (including the UK, USA, France, Spain, Hong Kong, Japan, S. Korea, and India) provided that the medication is for personal use, and it's not a controlled substance.
In practice, custom authorities around the world (including the USA and UK) have tightened up immensely on the importation of prescription drugs since the early 2000's. For example in Ireland the delivery of drugs will be automatically blocked by the Irish Tax and Customs service, and the package only released upon providing evidence of a prescription and the payment of VAT plus an administration fee.
Singer Dana International started hormones age c.17. It's unlikely they were obtained with a prescription.
Over the years many on-line pharmacies have been suggested to me as being prepared to ship hormones internationally without prescription, but this is a moving target and "buyer beware" is a vital consideration. E.g. Pharmacy Care New Zealand was an excellent source for several years, before going off-line in 2001 and reappearing in 2003 as a scam. Another consideration is that prices have increased immensely over the last 10 years - trying to buy drugs without a prescription can cost many times more than with a prescription, with no guarantee you will ever actually get them.
As a result of the customs clamp down many online pharmacies have closed down or been closed down. For the brave, web sites that I believe still exist include:
| 4 Corners Pharmacy ( |
http://www.4cornerspharmacy.com
) - offers USA and UK telephone numbers, but ships from the Republic of Vanuatu. May require a prescription before shipping to some destinations.
| Pharmacy Network ( |
http://www.pharmacy-network.com
) - used to be closely associated with transgendered woman Crissy Wild. They claim to be based in Europe, India and the Far East (Malaysia?). Very expensive.
And for optimists seeking a non-prescription herbal solution:
Important Notes:
|
| I have not personally used any of the above companies, and make no personal recommendation about the quality of their service. |
|
| Be warned that the cost of drugs on these sites is often much higher (double, treble, ...) than what you would pay in a local drug store/pharmacy if presenting a prescription. I can only suggest that you shop around. |
|
| After a clampdown on the |
personal importation
of prescription drugs by the
FDA
, women in the USA face possible customs detention and non-delivery of their orders.
|
| Because of known customs problems, some of these companies may not take orders which require shipping to some countries (e.g. Sweden and USA). |
|
|

While the warnings cannot be emphasised enough, and they are certainly not a magical potion, hormones have nevertheless helped to transform the lives of a million+ transsexual women in a way that was unimaginable just 50 years ago.
|
My Experience
I'm no doctor and have to say that you really should seek proper medical advice and supervision before starting hormone therapy, also it's essential to remember that some of the physical changes resulting from long term female hormone consumption by a male are permanent - there's no easy going back. However, I know the reality is that many girl do go DIY, and indeed the hormone regimen I personally follow was self developed, it is based partly upon trial and error experiences since I starting to take feminizing hormones in 1994, and partly upon research dating back to 1997.
|
More Information
For those that want to learn a lot more about hormones, here are two good links:
Copyright (c) 2013, Annie Richards














 "Female" type fat deposit areas
"Female" type fat deposit areas