Surgical Options for the
Transsexual Woman
Additional chapters in This Section include:
Gender Reassignment Surgery
Orchiectomy for MTF Transsexual Women
Bilaterial Orchiectomy Atlanta
FFS Facial Feminization Surgery
MTF Transsexual Surgeries
Hormone Replacement Therapy for Transgender Women
Female Hormone Therapy MTF Transsexuals
Breast Development in MTF Transsexuals
MTF Transsexual Breast Enlargement
Breast Augmentation MTF Transsexuals
Lactation and the Transsexual Woman
Injecting Silicone for Transsexual Women
Brazilian Hips and Buttock Enlargement
Average Body Size MTF Transgender
Male and Female Skeleton Transsexuals
Treatment of Young Transsexuals
Puberty in Adolescents MTF Transgender
Treatment of Young MTF Transsexuals
Treatment of Intersex Infants
Androgen Insensitivity Syndrome
Female Physical Beauty Transgender
Transgender Female Beauty
Exercise, Fitness and Diet for Transsexual Women

Background |
|
In the perception of the media and the public, a male-to-female transsexual (MTF) is a man who's had sex re-assignment surgery (SRS, also often rather inaccurately called gender re-assignment surgery - GRS). SRS involves major surgical procedures by which the physical appearance and function of a man's genitalia are altered to those of a woman. But there are other options, there are for example many transsexuals who happily live, work and socialize as women, but who haven't had any surgery at all.
|
Christine Jorgenson, her 1952 sex-re-assignment is widely considered to be the first using modern surgical techniques.
|
Some Numbers
|
The first recognized SRS procedure only occurred in 1952, but numbers have grown rapidly ever since. A BBC report in 2007 suggested that there were 15,000 post-SRS transsexuals in the United Kingdom (1 in 4000 of the population), although this seems high for the date. Contrarily, the
Gender Variance
report of 2009 estimated that in the UK there were 10,000 transitioned transsexuals, 3,500 of whom had had SRS - of which 80% of were MTF, implying 2,800 post-operative transwomen.
|
In the United Kingdom, the National Health Service (NHS) performed 137 SRS operations (all MTF) in 2009 (compared to just 54 in 2004); another 90 were funded by UK health insurance companies; and the Gender Identity Research and Education Society charity estimates that at least 150 such procedures are paid for personally by the patient each year - these are usually performed overseas, most commonly in Thailand or the USA. I.e. a total of perhaps 380 UK residents had male-to-female surgery in 2009.
|
A photo from a UK transgendered woman. The NHS undertook her SRS, but wouldn't provide breast augmentation surgery as well.
|
|
But numbers are increasing dramatically - by up to 50% a year! In 2013 the NHS early 4,000 (80% MTF, a fifth of which were under age 18) in 2015. MTF SRS procedures a year, but this is still far short of demand. A significant number of British transwomen still go private (mainly to surgeons in Thailand) to avoid the long waiting times.
|
Based on trends, a reasonable guesstimate is that at least 1,000 UK residents had male-to-female sex re-assignment surgery in 2015. This leads to the projection that there are now probably 10,000+ post-SRS women in the country (including just a few dozen who had operations performed in the 1960's or even the 1950's).
|
However, the UK is just a very small element of a global picture, indeed it would be very surprising if the one millionth MTF SRS procedure hasn't already been performed.
|
|
Sex Re-assignment Surgery
|
Most surgeons will consider as eligible for SRS genital surgery a genetically male "woman" over the age of majority who has undergone at least 12 months continuous female hormonal treatment, and who's also successfully lived for at least a year full-time as a woman. However a surprising large number of women who fulfil these criteria do not immediately seek SRS, or any other genital surgery. The reasons for delaying or avoiding SRS procedures are very diverse, but include:
|
| It is |
irreversible
- if there is
any
uncertainty don't do it
| Lack of money for surgery. |
| Potential loss of earnings after surgery. |
| Happy as is, no strong desire or psychological need to have female genitals. |
| A homosexual sexual orientation. |
| An enjoyable sexual relationship as a pre-SRS woman (not the same as 'homosexual') |
| Pressure from a partner, family or friends. |
| A desire to preserve a reproductive capability. |
| A medical problem which prevents major surgery. |
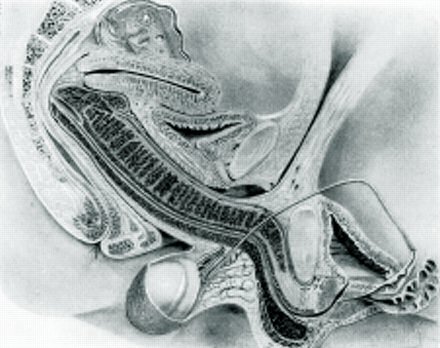
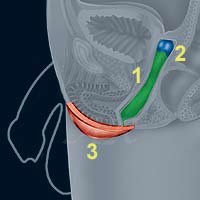
The Common "penis inversion" Male-to-Female Sex Change Procedure
|
|
|
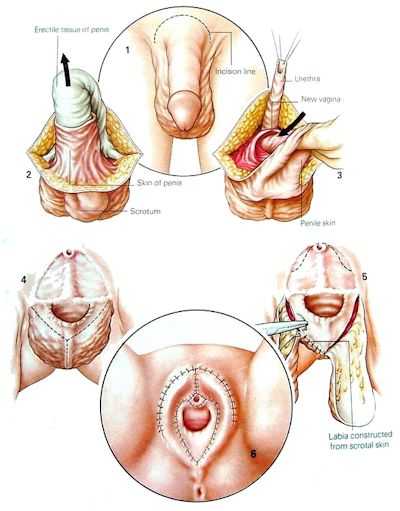
1. An incision is made around the base of the penis.
2. The skin is peeled back as intact tube and the erectile tissue is removed.
3. A vagina is constructed in the perineum and lined with the inverted penis skin.
4. The skin of the scrum is sectioned and the testes are removed.
5. The scrotum skin is used to make a labia, and the uretha is brought out and positioned above the vagina.
6. The operation is complete.
|
|
Unfortunately I haven't yet found any recent (rather than 1960's) statistics on the length of time after a real life transition until genital surgery for male-to-female- women, but I have found some interesting figures for female-to-males. Dr Holly Devor when researching her book FTM: Female-to-Male Transsexuals in Society found that most transsexual men retain some very dramatic physical manifestations of their previous lives as females. More than 1/3 of the 35 participants in her research who discussed this issue said that they began living as men without the aid of either hormone therapies or surgeries. Another 60% of them began their lives as men with the assistance of hormone therapy but, on the average, they did not have their first surgeries for another 3 1/2 years. Only six (15%) of the 39 transsexual men interviewed had had any kind of genital reconstruction surgery. Furthermore, despite the fact that they averaged 6.5 years since beginning hormone therapy, and 7.9 years since beginning to live full-time as men, slightly more than half (51.5%) of those who had not yet had genital surgery said that they were not particularly interested in having any done.
|
These extraordinary results are not directly relatable to transsexual women as much more difficult and expensive surgical procedures are required for female-to-male sex re-assignment than for male-to-female sex re-assignment. However they do reinforce my own belief that a medium [average] delay of 3 years from full time transition to MTF SRS would probably be near the mark, high though this may appear at first sight given that a common complaint from transsexual women is the need to wait a whole year after transition before being eligible for surgery.
Sexual desire can become a powerful motive for SRS...
... as can be presenting a female physical appearance when nude. [Breast augmentation scars are just visible below the areola]
But the reasons to have some form of genital surgery often strengthens with time, and most transitioned transsexual women eventually undergo some procedure. Possible drivers may include:
|
| A powerful desire to finally match the bodies physical sex with a female psychological gender and social lifestyle. |
| To present a female physical appearance when nude, and remove fear of identification as a "man" due to the presence of male type genitalia. |
| A desire to have 'normal' heterosexual intercourse with men as a woman. |
| Pressure from a partner, family and friends. This "encouragement" can be excessively strong after a transwoman admits her transsexuality and transitions |
| Fashion and Comfort - Tight and revealing clothes no longer present the "strange bump" fear. No more genital tucking and taping, or the discomfort of a gaff. |
| To remove the masculinizing physical effects and/or urges caused by the testes. |
| Health - Concern about long term liver damage due to prolonged use of anti-androgens and high estrogen and progesterone doses. |
| A strong and sexually exciting desire to have female genitals (a controversial reason). |
| To help a homosexual "man" have sexual relationships with attractive heterosexual men (a very controversial driver). |
The importance of the second point can not be underestimated. Post-transition but pre-SRS girl gradually collect bad experiences, ranging from embarrassment during a security check, a friend who sees too much, the wandering hands of a drunk, to the possibly fatal disappointment of a rapist.
|
|
Leslie - a post-SRS star of the dubious 1978 film "Let Me Die a Woman", which if nothing else demonstrates how truly desperate people can get for surgery.
|
|
Another rather depressing, driver that is now sometimes cited is homosexual men seeking to have sex-change surgery because it has become socially and legally more acceptable to be openly transsexual than openly homosexual (note: this reason must not be confused with the unpopular
homosexual transsexual
theory).
|
Age at SRS
A BBC report in 2007 claimed that there were 15,000 transsexuals in the United Kingdom (1 in 4000 of the population), and that they had a SRS at an average age of 29 - although this seems a surprisingly young age. |
|
Even today, half a century after Christine Jorgenson, most empirical evidence and published studies indicate that a majority of European and North American transsexual women are in their 30's, and 40's before they actively seek to resolve their gender issues. Inevitably this means that the patient age profile of surgeons undertaking sex-re-assignment surgery follows this trend - with a lag of a several years representing the time from the woman commencing treatment to having some form of genital surgery.
|
Shemale prostitutes during a "Gay Pride" march|
.
|
A chart showing the age of legal change of status (usually after SRS) of 712 German transsexuals aged 18 to 79. The average (mean) age is a 34.
Source:
Weitze C., M.D., Osburg S., M.D. (1997)]
|
Considerable publicity often surrounds
young transsexuals
who with the support of their parents transition and have surgery at a very young age - in their teens or early 20's. There is no doubt that this group is becoming more numerous, but it is still only a very small proportion of the transsexual community.
There is also a statistically significant group of young transsexual women (often from parts of Asia and Latin America) whose career in the sex industry leads to various surgery procedures in during their teens and 20's, but this is usually in the form of breast augmentation and facial feminization. When (or if) they finally decide to have SRS, typically in their 30's, it generally marks their move out of the sex industry.
|
|
The story of Vonlee (formerly Harry) Nicole Titlow shows the desperation of some transsexuals trying to fund their surgery. She's shown (age 33) during her trial for murdering her uncle for money.
|
|
Whilst the numbers are small, the general picture that a majority of western transwomen undergo SRS in or near their middle age is undoubtedly correct, for example an American
study
of 232 transwomen noted that their average age at the time of surgery was 44, with a range of 18 to 70. Similarly in the UK, the average patient age for 137 SRS procedures performed by the NHS in 2009 was 42, and only one patient was under 21. Cost is often a big issue, but the typical Asian transwoman seems to be able to find the money and will to have SRS at a least decade before the typical Westerner does. The huge difference in the age profiles of Asian and Western transwomen deservers further research.
|
Surgery Options
The transsexual woman who has transitioned full-time faces a difficult choice between a number of medical options regarding surgery on her male genitalia. In order of increasing complexity and cost these are:
|
| No surgery (although prolonged |
female hormonal treatment
will shrink the male genitalia significantly and will eventually cause permanent chemical castration after about 6-12 months use)
|
| Surgical Castration |
or Bilateral Orchidectomy, i.e. removal of the testes (or gonads) along with the undesirable masculinising and virilizing effects caused by the testosterone they produce.
| Chanelle, post-SRS. She now works as a model. |
|
SRS - removal of the testes and penis and the formation of female appearing external genitalia, but with no emphasis on vaginal depth. This is usually followed by a labiaplasty several months later.
|
| Full SRS with vaginoplasty - removal of the testes and penis and formation of female appearing external genitalia, formation of a neo-vagina with adequate depth for intercourse. Again this will often be followed by a labiaplasty. |
|
Figures and statistics are hard to find, but as many as 50% of all transitioned transsexual women may fall in category one, and some will never progress to another category.
|
The decision on which option to select is a personal choice that may well evolve over time. For example most men who believe that they are transsexual will start off assuming that they will have SRS as soon as possible when they seek treatment. However, after they have benefited from hormones (etc.) and perhaps transitioned to live as a woman they may no longer see any urgent need for SRS and it’s only some event years later such as a relationship with a heterosexual man that eventually causes them to have SRS.|
If there are any doubts, the best route is always NO surgery. It’s always possible to have surgery later, but it’s impossible to reverse castration or SRS. Even if surgery is decided on, the prior freezing of a sperm sample (if obtainable) may be a sensible measure to help preserve some reproductive options - even as a
mother
)
|
Castration is most commonly performed with intersex or gender disordered children, but some transsexual women do find it to be a useful and cheap halfway house to full SRS.
|
SRS always involves the formation of the entrance to neo-vagina (i.e. an artificial vagina). However for various reasons this can be often be quite shallow (just 2-3 inches, 5-7cm). The decision as whether or not to have a deep vagina suitable for intercourse is actually a decision which need not always be an automatic "yes" - particularly for elder women who perhaps don't intend to lead an active sex life after surgery.|
|
|
Natasha after having her SRS
For satisfactory penetrative sexual intercourse with a man a stretched vaginal depth of at least 6 inches (15 cm) is required, while this is about the mean depth of the neo-vagina of transsexual women, inevitably some women are shallower and this is a major cause of dissatisfaction in the result of SRS.
|
|
For accommodating intercourse with a well endowed male partner, a vaginal depth of up to 9” (20-22cm) is necessary. This is actually a very considerable depth which is rarely achieved in SRS, it either requires generous penile skin to be present (rarely the case with a MTF transsexual after prolonged female hormonal treatment), or scrotal skin (which requires painful electrolysis beforehand) or colon grafts be used to extend the depth - and even then the internals of the transwoman may be unsuitable for such a deep and broad cavity. On the other hand, most genetic women would also have problems fully accepting such a lucky man! It should also be remembered that reaching and then maintaining full vaginal depth requires the effort of regular dilation and/or then frequent sexual intercourse.
|
For SRS a variety of techniques are used, by far the most common is variations of the penile inversion method, while a rather less common method is variations of the sigmoid colon section method. An interesting debate about the merits of two methods can be found
here
, but accepted pros and cons can be summarized as:
|
|
Colon Section
|
Penile Inversion
|
Advantages
|
|
| Natural-looking neo-vagina. |
| No neo-vaginal contractures. |
| The fluid secreted from the intestine acts as a natural lubricant during sexual intercourse. |
| Desirable from the functional aspect of neo-vagina. |
| Only moderate neo-vaginal dilation required. |
| No risk of vaginal hair growth. |
| A relatively simple surgical procedure which greatly reduces possible. complications and related side effects. |
| No risk of causing peritonitis or intestinal adhesions associated with colostomy. |
| Rapid recovery - 4-6 days in hospital. |
Disadvantages
|
| It's major surgery that affects a healthy colon. |
| Prolonged recovery period due to an extensive surgery through abdominal cavity. |
| May develop complications such as peritonitis, intestinal adhesions and necrosis of intestinal graft. |
| The vagina may "leak" and smell. Sanitary pads in the panties can be a permanent requirement. |
| Painful electrolysis of scrotal hair is recommended by most surgeons. |
| Requires frequent neo-vaginal dilation. |
| Possible neo-vaginal contractures after surgery. |
| Sexual intercourse requires an artificial lubricant (KY Jelly et al). |
| Will need to douche daily to avoid an unpleasant vaginal smell and infections. |


The vulva on the left was a runaway favourite in a
survey
of transsexual women. Note the minimal amount of hair, the small clitoris, and the generally slight and delicate features. The vulva on the right is a post-operative result by a leading surgeon taken from the
Transsexual Women Resources
website.
|
Another medical debate is whether the lining of a neovagina gradually changes to that of a normal female vagina (technically a nonkeratinizing mucosal type squamous epithelium)
|
The anecdotal evidence of many transwomen indicates that in the months and years after a penile inversion, the skin graft slowly loses its skin characteristics and adapts to its new environment, taking on the characteristics of a normal vagina - including normal vaginal PH levels, complete loss of hair, complete loss of pigment, complete loss of sweat glands, and normal vaginal epithelial glycogen levels. Also, lubrication is rarely a long term problem with a neovagina - whilst it may take slightly longer than with a "natural" vagina, the most neovagina of most transwomen will self-lubricate when she becomes sexually excited.
|
Overall, it seems that the cells lining a neovagina slowly alter in type, and it's eventually impossible to distinguish between cells collected from the vaginal smear of a genetic woman, and that of a long time (10 or 20 years) post-operative transsexual woman. However at least one formal
medical study
has concluded that no significant changes occur, so the debate remains active.
|
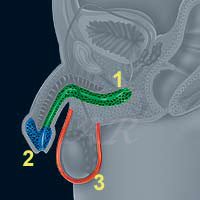
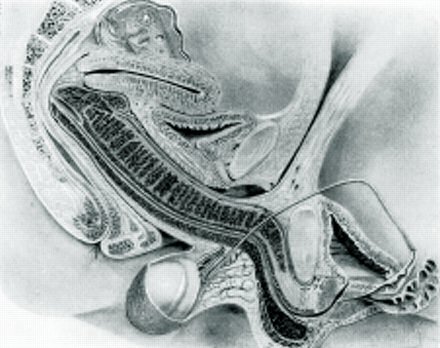
Overview of the Male-to-Female Sex Reassignment Surgery (Vaginoplasty)
Penile Skin Inversion Procedure
|
|
|
|
Before
|
After
|
|
1) An incision is made on the scrotum and the testicles removed. Most of the penis is amputated, but the skin and nerves are carefully preserved.
2) A vaginal cavity is made, the skin of the penis is turned inside out and used to cover the inner parts of the neovagina. The very sensitive glans goes deep inside and acts like the cervix of the uterus.
3) A clitoris is constructed from sensitive erectile tissue taken from the penis (some surgeons use a small part of the glans), and the scrotal skin used to build the labia majora.
4) A later labiaplasty may sometimes be needed to "tidy things up" and hood the clitoris.
With a good surgeon, the final aspect should be indistinguishable from real female genitalia.
|
|
|
The following factors will influence the results of the SRS and the depth of the vagina:
|
|

Bianca Magro had the first legal sex re-assignment operation in Brazil.|
|
| The patients body size (the smaller and lighter the better) |
| Circumcision (preferably not) |
| Length of penis (the longer the better) |
| Circumference of penis (greater the better, ideally more than 3 inches / 7 cm when 'excited') |
| Amount of scrotal skin (the more abundant the better) |
It is important to re-iterate that the prolonged use of hormones and an orchidectomy has a very negative effect in relation to SRS as in time the penis and scrotum will atrophy to some extent, i.e. the penis size reduces and the scrotal sack shrinks. The earlier that SRS is performed (ideally before hormones are even started!), the better the likely result, indeed some leading surgeons who are anxious to preserve their reputation are reluctant to perform surgery on a patient who has previously had an orchidectomy. Of course this situation contradicts the recommendation of many psychiatrists that a lengthy "real life test", usually associated with a hormone regimen, is essential prior to any genital surgery.
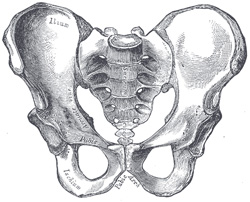
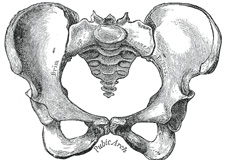
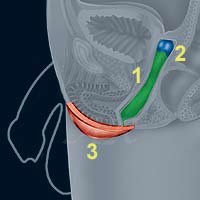
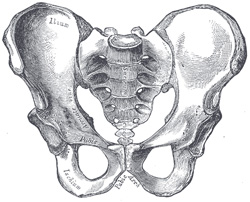
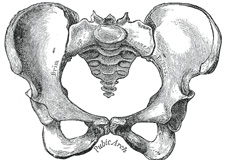
Top is a drawing of the front of a male pelvis, in the middle is a female pelvis. Bottom is a drawing of a female vagina accommodating a penis during intercourse, it's just possible to see how the penis is confined by bones, shown are the pubic arch bones at the front and the coccyx bones at back. This can be an uncomfortable constriction for a man penetrating the vagina of transwoman whose male type skeleton is not designed to receive a penis in the "missionary position".
|
|
For successful intercourse, arguably sensitivity and even appearance (it's 3:00 am, dark, 5 pints and a bottle of wine consumed ...) are less important than the fact that the neovagina feels totally natural to the man, particularly if the woman is stealth. Adequate depth is just one factor, others include adequate lubrication and the woman’s internal anatomy.
|
In general genetic women (regardless of their height) have broad hips, i.e. a broad
pelvis
with a pelvic cavity offering plenty of internal volume. They also have a wide pubic arch and a large oval-shaped pelvic inlet – ideal both for giving birth and for sexual intercourse. The result of this
skeleton
is that even an otherwise petite woman can comfortably and enjoyably accommodate a large penis. Unfortunately arrangements don’t tend to be quite so satisfactory for transwomen, who will have the skeleton of an XY man unless they began female hormones by early puberty. In general transwomen have a narrow pelvis, a tightly angled pubic arch, and a small, partially obstructed, heart-shaped pelvic inlet. For the majority of transwomen their skeletal structure would theoretically rule out natural delivery of a baby, and rather more relevantly the pelvic bone structures of a minority may unnaturally impede or even obstruct a penetrating penis, and also restrict the degree and direction that a neovagina can stretch to accommodate the penis.
|
Another issue is that fact that genetic woman have a strong muscular and ligament framework surrounding their vagina - muscles which act upon the penis during intercourse whether controlled consciously or unconsciously. Transwomen do not have any true vaginal muscles after their SRS – however a combination of determined will-power, constant (i.e. when ever possible through-out the day) internal exercising, and an active sex life can produce good results, e.g. the partner of one transwoman stating his great satisfaction with the vaginal muscular control that his wife had developed 18 months after her surgery.

The labelled upper picture shows the vulva of a typical genetic woman, the lower that of a transsexual woman. In general genetic women have a slightly higher placed, more delicate but less 'tidy' vulva.
|
Normal female appearing external genitalia can actually be constructed with little "material" to work with. Indeed it is worth pointing out that with modern techniques a good surgeon will usually produce a vulva that's more text book "female" in appearance than most genetic women actually have! An increasing number of genetic women (particularly in the sex industry) are apparently seeking plastic surgery to "tidy up" their external genitalia to a similar standard.
|
The external cosmetic problems - even with good surgeons - tend to relate to scaring, a slightly high vulva/vaginal position (usually due to skeletal limitations) and a rather too 'robust' appearance.
|
Vagina Not Required
Many transsexual women have SRS with little or no expectation of subsequent sexual intercourse. Indeed - base on limited evidence - about one in six post-SR women have never their vagina 'penetrated' during sexual relations.
|
This 'penis/dildo penetration not required' approach should perhaps be more common than it is as it offers the transwoman significant health and hygiene benefits - possibly too many surgeons and patients focus excessively on the creation of a deep neo-vagina which may not be necessary.
|
If a transsexual woman does not plan to have vaginal penetrative sexual intercourse then clearly there is no need to have a deep vagina formed, and unnecessary surgical procedures can be avoided and the subsequent dilation effort also will be spared.
|
The emphasis can instead be place on achieving the best possible external appearance, rather than on sexual functionality and enjoyment. For example surgeons find it difficult to construct from a penis a sensitive clitoris of natal female size and thus often have to balance sensitivity with avoiding excessive size - this conundrum disappears if 'good sex' as a woman is not a driver for SRS.
|
[Since first writing this, one girl has contacted me expressing her regret at not seeking and working for the maximum possible vaginal depth during and after her SRS], Conversely, if sexual intercourse and sexual genitalia able to accommodate deep penetration in the Missionary Position by even "Mr Big" are an immediate high priority, the colon section procedure may be preferable to the more common penile inversion technique despite the risks and complications as it provides a more convincing looking, self-lubricating and self-cleaning neo-vagina, and arguably copes better with frequent and robust penile penetrations.
|

Scans of the pelvic region are used to design a tube like 3D-scaffold for each patient, the vagina is then built on this.
|
The Future
A serious possibility for the future is that transsexual women may be implanted with female sexual organs grown from their own cells. For example, a report in a 2014 edition of the medical magazine Lanclet described how four women (all teenagers) born without vagina's had had new vaginas grown in a laboratory and implanted by doctors at the Wake Forest Baptist Medical Centre in the USA.
|
The women's vaginas did not form properly while they were still inside their mother's womb, a condition known as vaginal aplasia. Current treatments normally involve surgically creating a cavity, which is then lined with skin grafts or parts of the intestine - transsexual women essentially undergo the same surgical treatment.
|
Under the new procedure a tissue sample and a biodegradable scaffold are used to grow vaginas in the right size and shape for each woman - as well as being an exact tissue match. After surgery, the woman all reported normal levels of "desire, arousal, lubrication, orgasm, satisfaction" and painless intercourse.
|
Caveat Emptor - Buyer Beware
It was the 1976 when first started to wonder if I was a transsexual (transgender and suffering from gender dysphoria in modern terminology). At that time only a few clinics (E.g. the John Hopkins Gender Identity Clinic) and surgeons (most famously Dr Georges Burou in Morrocco) were performing sex-reassignment-surgery, perhaps a few hundred operations per year world-wide. Fourty year later there is
|
|
Regrets
While most post-operative transsexual women don't regret their decision (or claim they don't), a few do - and this fact cannot be ignored.

Sam Hashimi became Samantha Kane, who is now Charles Kane
|
C: "If I had been properly assessed, it would have been obvious that sex-change surgery was inappropriate for me, I was desperately unhappy and was going for a sex change because I felt under pressure from my boyfriend. I'll never have a relationship. Who's going to want me when they could get a real woman? I am not a woman, I am a sex change, and men know that. I fundamentally regret having had surgery. I could have lived as a woman without mutilating my body, but no one talked to me about the possibility."
|
M: "If and when you have [SRS] your life will be forever changed, in more ways than you can possibly imagine and anticipate. Being a woman is no better than being a man (in fact, in many ways it's a lot worse) - you just have a new set of problems. For me, being a woman expressed who I really am, but sometimes I think the cost of that self-expression was too dear."
|
W: "Becoming a woman has been a disaster, this experience has ruined my life. I felt excited when dressing as a woman but looking back it messed up my head - [psychologists] had me believing I'd always wanted to be one. [After SRS] I tried to persuade myself I had no regrets. [A] reversal won't solve all my problems, I will still be tortured by what I gave up to become a woman."
|
Samantha Kane: "The whole experience was very distressing for me - it was a devastating operation and very difficult. I was a heterosexual male - I have never been gay - and that is why it didn't make any sense to have [SRS]. I was suffering from a nervous breakdown after the break-up of my marriage so I was very upset. I took hormones which changed my mind and my body so I wasn't thinking clearly. After the surgery my mind was a lot clearer and I felt better ... I wanted to live back as a man because I knew I wasn't a woman." Samantha also found that having sex with her boyfriends was boring, and that she had "penis envy".
|
More Information
|
For the very interesting results of a Post-Operative Survey of Transsexual women, see
here.
|
For a dire warning about the risks of low cost, back street, SRS, read this
article
.
|

Dr Carlos Cury (centre) with some of his post-operative transsexual patients in a photograph for the Brazilian magazine "Hands". His secretary, Guta is in the white dress to the left of Dr Cury.
|

Guta Silveira was one of Dr Cury's patients, and is now his secretary.
|
Copyright (c) 2004, Annie Richards